The health-care equation: Value = Quality + Patient Experience + Cost
Iowa hospitals, insurers work to rewrite the formula for delivering care

Under a new model of care known as accountable care organizations, Iowa hospitals and health insurance companies have entered into agreements in which they will track specific quality measures and quantify how patients rate the care they receive. The providers that meet those criteria will be eligible to keep a portion of the savings in health costs that are generated by taking care of the total populations more effectively.
Iowa’s leading health-care systems are rolling out a new care-delivery and payments model – one they believe will enable them to improve the quality of patient care and, in the process, reduce the rate of increase in health-care costs.
It’s a new formula for health-care value that considers quality, the total patient experience and cost as key components.
Through that model, known as accountable care organizations (ACOs), Iowa Health System and Mercy Medical Center – Des Moines plan to proactively reach out to entire patient populations to help them better manage their health, with a goal of keeping people healthy and out of the hospital. And the state’s dominant health insurer, Wellmark Blue Cross and Blue Shield, will provide incentives for achieving those cost-saving goals.
More health care reform coverage
Mercy and Iowa Health in April entered into separate but identical agreements with Wellmark to launch ACOs. Under those ACO payment models, Wellmark agreed to share cost savings achieved by the health systems, provided they meet specific quality standards.
From a health insurance perspective, the move to ACOs is a 180-degree shift from the traditional pay-for-performance model that pays health systems based on the volume of procedures performed to a patient-based, value-driven approach, said Laura Jackson, Wellmark’s executive vice president of health-care strategy and policy.
“The real story is going to be in a couple of years, when you have (a hospital administrator) sitting in front of you saying, ‘We’ve bent the cost curve, and we did it through quality and our patients love us,’” she said.
Iowa Health
Iowa Health’s chief executive said his organization realized an ACO-type restructuring was needed, regardless of the direction federal health reform takes.
The ACO “is fundamentally in response to our assessment, and Wellmark’s assessment, that the current system needed to change,” said Bill Leaver, president and CEO of Iowa Health System, “It is certainly spurred by the (federal health-care) reform legislation, but I think we’d certainly be talking about something different even absent reform, because in part, our customers are demanding that.”
Iowa Health has been working with Wellmark for the past two years to develop its ACO, Leaver said.
“What we have come up with is a multiyear contract that changes how Wellmark will pay us for care and (establishes) agreed-upon quality metrics,” he said. “So it’s not just about cost; it’s about patients and the quality outcomes we’re going to produce. But the focus will be on reducing that rate of inflation in medical spending, and the ultimate result, I believe, is that costs will go down.”
Under the current health insurance system, Wellmark reimburses medical providers on the basis of volume, not quality, Leaver noted. That payment system leads to doctors scrambling to see as many patients as possible, overflowing emergency rooms and escalating costs.
“You have to break that cycle, and that’s what this contract does,” Leaver said. “It starts to incent physicians and hospitals, with our home-care entities wrapped around that, to get rewarded when we keep the patient out of the hospital.”
Initially, Iowa Health will roll the ACO model out in four of its markets in Iowa – Cedar Rapids, Des Moines, Fort Dodge and Waterloo – and will begin by focusing on patients with chronic diseases. Iowa Health’s Fort Dodge hospital group is also part of a “pioneer” test of a Medicare ACO model. Both Iowa Health and Mercy have also applied to launch ACOs for their Medicare patients.
“The redesign of the care system that’s centered on the patient has been going on for three years,” said Dr. Alan Kaplan, vice president and chief medical officer for Iowa Health.
Through the remainder of 2012, Iowa Health will focus on reaching out to patients with chronic conditions, such as congestive heart failure and diabetes, which make up 5 percent of its patient population but generate 50 percent of health-care spending, Kaplan said. That focus won’t be to the exclusion of prevention and wellness, however.
“We have quality metrics focused around appropriate immunizations and screenings, for instance, to make sure we catch cancer earlier when we can cure it at lower cost and better outcomes,” he said. “And we are looking at patient satisfaction, to ask if they have access; did the care team answer your questions and provide good service?”
Mercy
Mercy Medical Center’s ACO, which takes the same type of quality-based approach as Iowa Health’s, will focus initially on people with two or more chronic illnesses, said Dr. David Swieskowski, Mercy’s chief accountable care officer. Most important, the health system’s priorities will now be aligned with Wellmark’s incentives.
“The issue prior to the ACOs was, if you put a wellness program together for your patients, no one pays (the health-care providers) for that,” he said. “These programs are not cheap. So under the old model, we would have to put the program together at our own expense, and get no reimbursement for it. The result would be that we would reduce hospitalizations, so we would lose even more revenue.
“With the ACO contract, if wellness counseling leads to healthier people that don’t end up in the hospital, then we have savings that fall back to us. It changes the incentives for us. It allows the providers of care to decide what’s going to be the best use of funding, rather than the insurance company decide how best to fund things.”
Both health systems have developed new mechanisms for better coordinating patients’ care. Mercy, for instance, is using a multifaceted approach to improve the flow of information about patients, Swieskowski said. A key element will be a recently launched patient registry that will provide doctors with a picture of an entire patient population, not just the ones who have come in recently to be seen.
Known as a patient registry or data warehouse, Mercy’s new MedVentive system pulls patient data from Mercy’s billing system, electronic medical records, laboratories and pharmacies and puts it into one database. “So one, we can know who has two or more chronic diseases, and two, we can know who’s overdue for care and who is not meeting their goal, (such as) who with high blood pressure doesn’t have their blood pressure controlled,” Swieskowski said.
Additionally, Mercy has defined at a more granular level doctors’ responsibilities for what have been gray areas of care so that, for instance, a primary care doctor and cardiologist are clear on which of them should follow up on a particular condition, such as high blood pressure. Until now, more than one doctor might be keeping tabs on it, or no one might be tracking it, Swieskowski said. “And we’re going to track it electronically to hold those specialties accountable and make sure they’re doing it for the entire population.”
Mercy – Des Moines is serving as the pilot ACO for Mercy Health Network, which is made up of 38 Iowa hospitals that are owned or affiliated with the health system. Mercy officials said planning is under way to launch ACOs at other hospitals within the health network, but a specific timetable hasn’t been established yet.
To assist the doctors in better managing their patients’ health, Mercy will use its existing team of 28 health coaches, who will use the data to follow up with patients in setting goals and designing plans to achieve their health goals. By the end of the year, the patient registry will be able to input patient data automatically, freeing up the health coaches to work more closely with patients, Swieskowski said.
Iowa Health’s equivalent of health coaches are known as the “advanced medical team,” Kaplan said.
“With this (team), our physicians have access in a single phone call to a nurse that’s specially trained in integrated chronic care disease management,” he said. “That nurse will go to the home and do a full assessment of that patient and put a care plan and health system resources around that patient, in coordination with the family and the primary care physician, to take care of that patient in a way they have not had access to care before..”
Wellmark’s Jackson said it will take time for the ACO models being adopted by the health systems to have an effect on premiums.
“I think it’s going to take a couple of years to see the way that the system works and ultimately result in reduction in claims costs that can be underwritten in a product,” she said. “So our goal, hopefully by two or three years, is that we could actually see the rate of inflation in health-care costs equaling somewhere near the Consumer Price Index on a rolling three-year average.”
Reducing the rate of increase in health-care costs to at least match the inflation rate has been a goal of Wellmark’s since 2008. Since then, there have been “pockets” of success toward that goal, Jackson said.
“We have actually seen employers that have leveraged benefit design with no increases in premiums, that have been keeping their costs flat,” she said. “We have seen some of our products actually experience a negative rate increase. But I think absent engaging a system like Iowa Health System to really think about how you fundamentally change how care is delivered versus kind of nipping at the edges, we really didn’t have an opportunity to do something sustainable.”
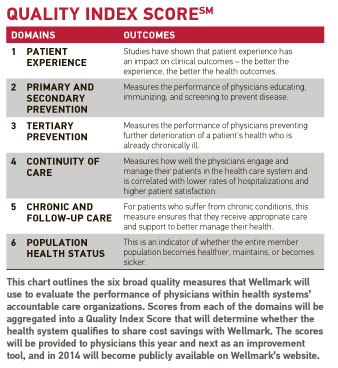
Under Iowa Health’s and Mercy’s identical ACO agreements, Wellmark has established six quality “domains” that include 18 quality measures, which together will be used to calculate an aggregate Quality Index Score for each physician and clinic group. Those scores will serve as the basis, or “trigger,” for whether the health system qualifies to share in cost savings with Wellmark.
Hospital leaders say they wholeheartedly support the quality measures that will be used.
“The quality triggers are fundamental things that should be done to improve the delivery of care,” said Eric Crowell, president and CEO of Iowa Health – Des Moines.
Mercy’s Swieskowski called the selection of the quality measures “a slam-dunk.”
“At Mercy, we’re very comfortable with quality measures; we’re very confident that we can improve them,” he said. “So any kind of measure of quality that we think is in the patient’s best interest, we have no problem saying, ‘We’ll do that one.’”
What’s next
Because the ACOs will not include any self-insured employers, which are typically the large-group plans for Greater Des Moines’ biggest employers, the ACO model will initially have a limited patient enrollment. For Mercy, Swieskowski estimates that only about one-third of its Wellmark-covered patients, primarily small groups and individual purchasers, will be part of its ACO. In terms of its overall patient population, about one in five Mercy patients will be covered by the ACO initially, he said.
The question of how Mercy treats its patients outside the ACO is a “big issue for us,” he said. “What do you do about people who are in the ACO versus people who aren’t in the ACO? Our mission is to help everybody. On the other hand, the ACO is paying for some expanded services that people outside the ACO aren’t paying for.”
Mercy has decided it will use its disease registry to track its entire population, which will enable it to determine whether the ACO patients’ overall health is improving relative to the entire patient population. Though ACO-covered patients will receive more comprehensive outreach through Mercy’s health coaches, Mercy will also connect a non-ACO patient with a health coach if a doctor or the patient requests one, Swieskowski said.
Both health systems say they plan to expand the coverage of the ACOs over time. Iowa Health, for instance, is working toward offering the same model in other markets throughout the state, Leaver said. However, it hasn’t yet determined how to incorporate the model into rural hospitals, he said.
Leaver said pundits have been quick to group the ACO model with other quality programs that have been tried and failed.
“Our view is that we have not tried it with a physician at the center, directing the care of the patient,” he said.
Swieskowski acknowledged there is no guarantee that the new ACO model will work. “It’s a little scary,” he said. However, successes of two of the nation’s largest health insurance plans, CareMore and Health Care Partners, suggest that it will. Mercy has studied the practices of both health plans, which focus on proactive, coordinated delivery of care to entire populations within their services areas.
“We think the way you’re going to reduce the cost of care is to improve the quality to the point where the people are not as sick; they’re not using the emergency and hospital services like they were, and that’s where you’re going to save money,” he said.