1.1.14 Health-Care Reform: How will health-care providers (and your care) be affected

Editor’s Note: Whether you agree with the law or not, health-care reform is coming. This is part three in a series exploring the effect of the reform on businesses, insurance companies and health-care providers.
Iowa’s health-care providers are on the front lines of a campaign to lower costs, improve quality and increase access to care.
Beginning next month, Iowa hospitals will start to see whether quality initiatives they’ve instituted in the past couple of years have been effective, as some significant changes to the Medicare payments systems from the Patient Protection and Affordable Care Act take effect.
Central Iowa hospital leaders say the federal health overhaul provided incentives for their organizations to move forward with initiatives that otherwise might not have progressed as quickly, the most significant being accountable care organizations (ACOs). Regardless of whether a Republican or Democrat is elected president this November, health leaders in Iowa say the momentum will continue.
The immediate effect?
Patients should start to notice a shift to a more holistic approach to health from their primary care doctors, although the focus at first will be on the most chronically ill patients. But don’t be surprised if you receive a telephone call or email or two from your doctor’s office in the next year, reminding you to come in for a check-up or following up on how well that medication you’ve been prescribed is working.

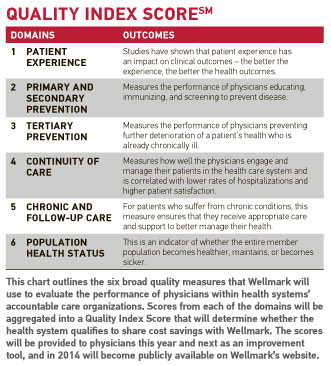
Central Iowa health-care providers took a major step toward a quality-based model of care in April, when competing health systems Mercy Medical Center – Des Moines and Iowa Health System entered into separate agreements with Wellmark Blue Cross and Blue Shield to form accountable care organizations or ACOs. Those agreements formalized a new type of payment model in which Wellmark agreed to share cost savings achieved by the health systems, provided the hospitals meet specific quality standards.
Those private-sector ACOs are modeled after Medicare ACOs, also known as the Medicare Shared Savings Program, that health-care organizations across Iowa are also participating in. Wellmark will base its cost sharing with the hospitals on six quality measures that take into account how well physicians are caring for and following up with patients.
Health-care leaders say the ACO models they are implementing are patient-centered initiatives that will not result in rationing of care as the failed health maintenance organization (HMO) model did in the 1980s.
“I’m definitely an advocate of paying for performance, paying for quality,” said Dr. Michael Kitchell, a physician at McFarland Clinic in Ames and past president of the Iowa Medical Society. “If we emphasize that our people need better quality care at a better price that doesn’t waste money on unnecessary tests, isn’t that what we really want?”
Various incentive and penalty programs enacted under the Affordable Care Act that apply to Medicare patients have prodded health systems to implement the broader ACO initiatives that could benefit all patients.
How ‘pay for performance’ works
On Oct. 1 Medicare’s pay-for-performance initiative will begin paying hospitals bonuses based on how well they meet 12 quality criteria, along with the results of hospital-conducted patient satisfaction surveys. The first-year bonus pool of $850 million was created by reducing overall payments to hospitals by 1 percent. The bonuses will increase by one-quarter of a percent each year, taking it to 2 percent of Medicare payments in October 2016.

Although the first measurement period for the bonuses ended in March, it’s difficult to estimate the net effect on hospitals’ Medicare reimbursements, he said. Overall, he guessed a net takeaway from Iowa’s hospitals of between $200,000 and $400,000 in the first year. “I don’t think there have been a whole lot of (hospitals) that have been winners out of this,” he said.
According to a study by leading health policy journal Health Affairs, nearly two-thirds of hospitals will experience changes of just a fraction of 1 percent through Medicare’s pay for performance bonus system.
“Although the program will in effect redistribute resources among hospitals, our data suggest that the redistribution is not likely to cause major problems because the amount being redistributed is also small,” the report said. “These results raise questions about whether the new pay-for-performance program will substantially alter the quality of hospital care, and they highlight the challenges of designing effective quality improvement incentives.”
If a carrot doesn’t work, then a stick might. Beginning Jan. 1, physicians must begin reporting quality measures and using electronic medical records to avoid a 4.5 percent penalty deduction from their Medicare reimbursements in 2015. That penalty will ratchet up to 8 percent over a seven-year period.
Targeting readmissions
Hospital readmission rates will also be under the spotlight as a criterion for penalties. Using three years of past data for each hospital for three key treatment categories – heart attacks, heart failure, pneumonia – hospitals will begin to incur penalties if their readmission rates increase for those conditions.
Iowa Lutheran Hospital in Des Moines, for instance, will have its Medicare reimbursements reduced by a factor of 0.36 percent, or less than four-tenths of 1 percent, due to its readmission rates in the past year.
Reducing readmissions can be a difficult problem to tackle, said Purtle, adding that Lutheran’s readmissions weren’t that far off from hospitals that had no penalty.
“Oftentimes it has nothing to do with the care provided or that they were discharged too early,” he said. “The reasons are often that their medications aren’t understood, or they may come home and start taking medications they still had on top of what they were prescribed. Or they don’t have the money and have to wait for their prescriptions. For someone with congestive heart failure, that can be quite an issue.”
The Affordable Care Act also has a value-based Medicare payment modifier for physicians, which will be based on the same 12 quality measures, or 29 measures for groups of 25 doctors or larger. Similar to the hospital bonuses, doctors will be able to earn bonuses for surpassing the quality standards. However, doctors who don’t implement quality measures and electronic medical records to enable them to share that data will face the 4.5 percent reduction in their Medicare payments in 2015.
“Unfortunately, only about 26 to 30 percent of physicians are reporting these quality measures,” Kitchell said. “Most physicians are too busy running on the treadmill to know about these programs. I think the large health organizations will be the ones to get their physicians on board.”
As changes unfold in the health-care delivery model, health systems will use technology to track patients across the spectrum of care and reach out to them more frequently.
Both Iowa Health System and Mercy Medical Center – Des Moines have invested millions of dollars in establishing and networking electronic medical records systems in an effort to reduce duplication and waste.
“This gives us the electronic ability to look across the continuum to see what has happened to the patient, so that you don’t have lost records and everyone knows what has been done,” said Marcia Stark, ACO director for Iowa Health – Des Moines.
Primary care physicians will play a greater role in the care of their patients, although it may be a nurse practitioner or physician assistant who sees patients for more routine matters, said Dr. Michael AbouAssaly, a family practice physician in Burlington.
“We’ll have to start to prioritize what (conditions) we can see what we can’t see – moving from seeing the whole family to (being) a chronic disease manager,” said AbouAssaly.
AbouAssaly, who was recently named Iowa medical director for Holmes Murphy & Associates to work with employers on strategies to lower their health-care costs.
As a doctor, he realizes the changes may reduce the level of control he has over how he’s paid, such as when Medicare begins bundling services under one price.
“The good thing about it is that it will force doctors and hospitals to provide the most efficient care possible,” he said.
Five questions to ask your doctor:
1. Does your doctor or staff coordinate or schedule appointments for all your health services (laboratory, x-rays, education, hospitalization, specialists)?
2. Does your doctor routinely recommend preventive care to you and provide you with 24-hour access to health information and medical advice?
3. Is there good teamwork, communication and information sharing between your primary care doctor, specialists and supporting staff?
4. Does your doctor seem well-informed about new treatments for your condition, and is your doctor able to help you evaluate the pros and cons of your medical options?
5. Does your doctor make use of health information technology, including electronic medical records, to share your medical information with the specialists you see?
Source: Council of Accountable Physician Practices
Medicare readmissions penalties – Iowa hospitals
These numbers show the percentages by which Medicare reimbursements will be reduced for these hospitals this fiscal year based on the hospitals’ readmission rates.
Broadlawns Medical Center: 0%
Iowa Lutheran Hospital: 0.36%
Iowa Methodist Medical Center: 0%
Mercy Medical Center – Des Moines: 0%
Trinity Regional Medical Center – Fort Dodge: 0%
St. Luke’s Hospital – Cedar Rapids 0%
Mary Greeley Medical Center – Ames 0%
Grinnell Regional Medical Center 0.19%
Mercy Medical Center – North Iowa, Mason City 0.14%
Iowa average readmission penalty (36 hospitals) 0.12%
Source: Centers for Medicare and Medicaid Services
Key dates for health-care providers
Oct. 1, 2012
• Medicare quality bonuses begin
• Standardized bill coding and electronic medical records requirements start
• Penalties begin for excess readmissions
Jan. 1, 2013
Increased Medicaid payments for primary care doctors take effect
• Medicare Bundled Payment pilot program begins
Jan. 1, 2014
• Medicare penalties for hospital-acquired conditions begin
Jan. 1, 2015
• Higher Medicaid payments to doctors based on quality measures take effect