New name, same role for Mission Cancer + Blood
Des Moines-based oncology and hematology physician group is behind-the-scenes MVP for cancer patients

JOE GARDYASZ Mar 26, 2020 | 6:27 pm
6 min read time
1,475 wordsBusiness Record Insider, Health and Wellness
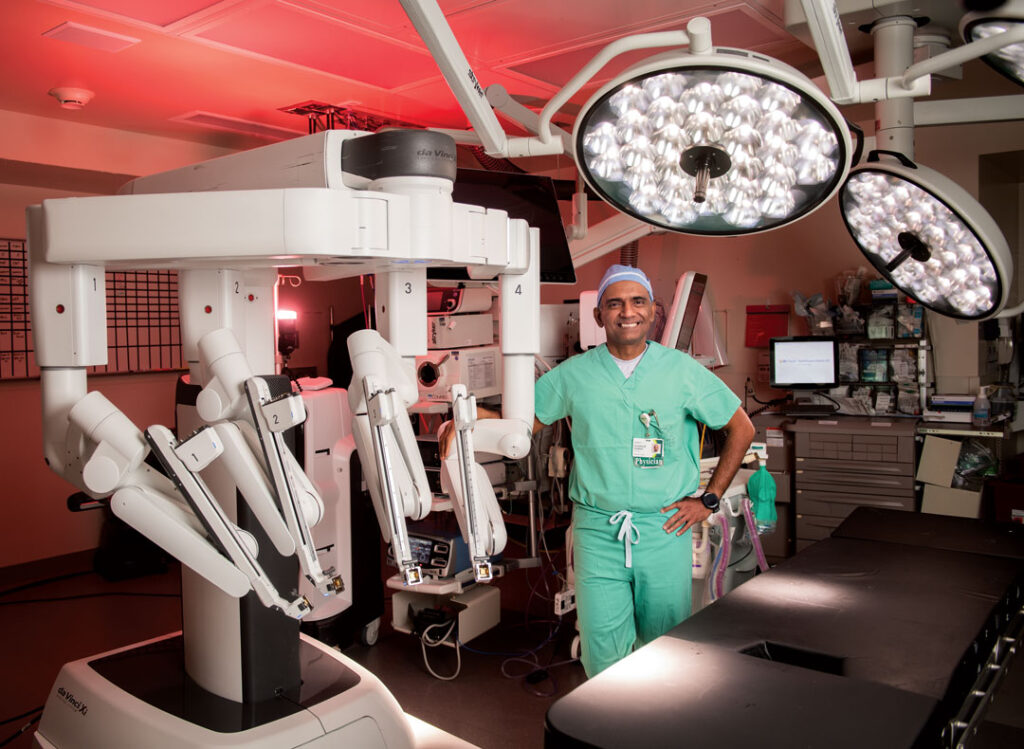
One of Central Iowa’s largest cancer medicine practices has two primary sets of stakeholders — the medical groups that it partners with and the patients that its physicians treat. For the latter group, however, many patients may not even realize that their oncologist is part of an independent physician group that’s been around for nearly 40 years.
Founded in 1981 as Medical Oncology and Hematology Associates — known as MOHA by the doctors — the Des Moines-based regional practice has rebranded as Mission Cancer + Blood. It’s among the largest privately owned community oncology and hematology groups in Iowa, with 21 physicians and 22 advanced practitioners. Along with a support staff at its Des Moines headquarters and nursing staff at the three cancer centers in Greater Des Moines and 22 satellite locations statewide, the organization has about 230 employees.
The practice has had long-standing partnerships with MercyOne Cancer Center and the John Stoddard Cancer as well as the Iowa Clinic, said Phil Stover, who joined the organization in 2015 as chief executive officer and its first professional, nonphysician administrator.
“We kind of operate behind the scenes of the centers, and that’s good — we want [the cancer centers] to be highlighted,” Stover said. “But we also want patients to know the underlying breadth and depth of expertise that they’re going to get right here in Central Iowa.”
The rebranding, completed last October, was really triggered by the need for a much-improved website, he said.
“As we were looking at the website, we said: ‘If we’re ever going to tackle rebranding, now’s the time before we invest heavily into the website.’ Our group had been known as MOHA and our website was Cancer Center of Iowa. A lot of our patients didn’t even know we are an independent group. And so all of those factors came into play in that there was a lot of confusion about who this group was, really.”
Community-based oncology services have been shown to provide significant cost savings to patients by providing cancer care closer to home, and it’s a beneficial arrangement that patients and their families greatly appreciate, he said.
“We love being there and being able to provide that service, and I think it’s a lot better for the employers too, because [their workers who are getting treatment] are in their hometown and recovering quicker.”
Stover initially connected with Medical Oncology and Hematology Associates as a consultant, when he organized the executive search for its first CEO. That process led to him unintentionally being selected as one of the top candidates to fill the CEO position. He became the board’s eventual choice for the new role, which he stepped into in July 2015.
The past five years have been largely a refinement of processes that were already guided by a successful practice philosophy, Stover said. That philosophy has been summarized by one of the group’s senior physicians as “the three A’s” — Available (for patients and referral partners), Affable (forming relationships beyond being a physician) and Able (being the best at what they do).
“Those three things really haven’t changed at all, which makes it easy for a new leader to come in, when the foundation of the attitude of what’s made us successful is really a good one,” he said.
One of Stover’s accomplishments over the past several years has been better coordinating the group’s operations for increased efficiency. The organization maintains 22 outreach sites across the state, along with locations at John Stoddard Cancer Center, MercyOne Cancer Center in Des Moines and MercyOne West Cancer Center in West Des Moines. Its corporate office — housing all administrative functions — is at 100 E. Grand Ave. in Des Moines.
The group has all of the available clinical trials for cancer treatments loaded into its system so that its doctors can immediately refer patients to suitable trials. An enhancement gained last year with Mission Cancer’s upgraded website: When physicians are reviewing a patient’s case on the computer, a banner will automatically pop up indicating any clinical trials that the patient may match with given their condition.
Mission Cancer + Blood has between 60 and 65 clinical trials open at any given time, with the majority federally funded through the National Cancer Institute, while the remainder are industry-funded through pharmaceutical companies.
“Both groups at John Stoddard and MercyOne are fantastic in providing a lot of different trial opportunities — there are just hundreds of them for different disease states, and so that’s something we’re pretty proud of,” Stover said. Notably, for the first clinical trial that came about as a result of then Vice President Joe Biden’s Cancer Moonshot initiative, the Des Moines practice registered the first patient in the nation for that trial.
There is often an information gap in patients not knowing about the clinical trials available very close to home, said Shannon Benson, administrator of the Iowa Oncology Research Association, which works with the John Stoddard Cancer Center at Iowa Methodist Medical Center.
“We will get patients who live in the Des Moines area but who traveled to Mayo Clinic to find out that trials are open here in Des Moines,” she said. “[They’ll be told]: Go back to Des Moines and see your physician there.”
One of the newest services that Mission Cancer + Blood now provides is a genetic counseling program to help determine whether patients can match with available clinical trials or are eligible to try newer treatments that are offered for patients with specific genetic traits. The practice has hired a full-time certified genetics counselor who is now seeing all patients who are referred to the group.
Looking ahead, Stover said he anticipates continued growth in the practice due to the growing number of aging baby boomers. Although the rate of people who are being diagnosed with cancer isn’t substantially changing, shifting demographics means more people who are more likely to have cancer as they get older.
“They say that there’s going to be a steady increase in cancer through 2035,” he said, “and so we’re always going to be recruiting.”
Genetic counseling now offered for cancer patients
In January, Mission Cancer + Blood added an in-house genetic counselor for the first time. It’s a relatively uncommon service for an oncology group to offer, said Ann Frankl, who had worked as a genetic counselor for UnityPoint Health-Des Moines for seven years before joining Mission Cancer.
In her prior position, she would see cancer patients along with a mix of other patients, but she decided she really wanted to focus on working with cancer patients. Then the opportunity to join Mission Cancer came about.
“We got real excited when we heard she had become available,” said Phil Stover, CEO of Mission Cancer + Blood. Genetic testing and counseling will continue to play a larger and larger role as researchers learn more about different types of cancers, he said. “So it’s one of those lines in our practice that I can just see growing with the need for this, and I can see her eventually overseeing others as the need grows.”
Patients with breast cancer and colon cancer are two of the cases most frequently referred to her, as they are among the most common diagnoses. “We know that about 5% to 10% of patients will have their cancer related to a genetic predisposition that they were born with,” Frankl said. “So generally I’ll see patients who are young, who have a strong family history [of a type of cancer] or who might have a tumor type that’s suggestive of a genetic predisposition. So there are some specific ones that look more genetic than others.
Once someone has learned that they have a certain genetic factor, it can sometimes influence what therapies are chosen. It might also change how frequently a patient returns for screening or the preventive options taken to reduce the risk of cancer returning. The testing also provides insight for family members to know their risk of getting cancer.
On average, about 10% of patients tested will come up positive for a genetic mutation that’s related to an increased risk of cancer, Frankl said.
“So still the majority of cancers aren’t related to what we know about underlying genetic predispositions,” she said. “But it’s important — at least in the higher risk patients; there are a lot of criteria out there that establish who is appropriate for genetic testing — knowing that we try to cast a wide net to catch everyone who might have a genetic predisposition and the majority of people will test negative.
“But they still could have some familial risk, given their family history that we might still want to adjust their screening protocols, or they might still be at higher risk of cancer [and] we just don’t have a solid genetic explanation as to why.”