Obesity presents significant economic challenges in Iowa, new report shows

Obesity is not only a chronic disease that 36.4% of Iowans currently live with but also a significant economic challenge that affects nearly everyone, according to findings from a new study by GlobalData PLC.
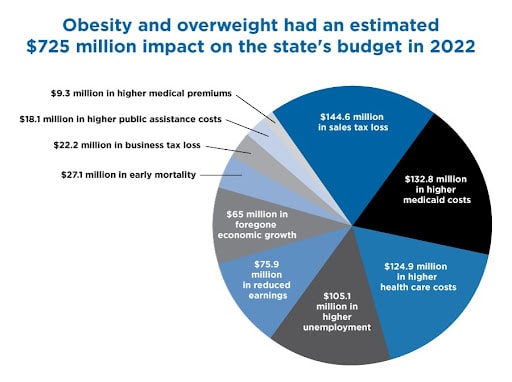
The “Obesity’s Impact on Iowa’s Economy and Labor Force” report found that for 2022, excess weight and obesity reduced economic activity in Iowa by $5.7 billion, which is equivalent to 2.5% of the state’s 2022 gross domestic product. The effect on the state budget was $725 million, which is equal to 5.9% of 2022 fiscal year revenues, with state tax revenues lowering by $449.2 million and state costs for Medicaid, public assistance and state government health insurance increasing by $275.8 million. Additionally, $415 million was attributed to health-related absenteeism and disability costs due to obesity or excess weight.
A body mass index (BMI) over 25 is considered overweight, and over 30 is obese, according to the World Health Organization. Body mass index is a person’s weight in kilograms divided by the square of height in meters.
Nationally, 41.9% of adults have obesity, according to the 20th annual State of Obesity report by Trust for America’s Health (TFAH). Black and Latino adults have the highest obesity rates at 49.9% and 45.6%, respectively. Nearly 20% of children and adolescents between the ages of 2 and 19 have obesity, according to 2017-20 National Health and Nutrition Examination Survey data.
“It’s critical to recognize that obesity is a [multifactor] disease involving much more than individual behavior,” J. Nadine Gracia, president and CEO of Trust for America’s Health, said in a prepared statement. “In order to stem the decades-long trend of increasing obesity rates, we have to acknowledge that the obesity crisis is rooted in economic, health and environmental inequities. Ensuring all people and communities have equitable opportunity and access to healthy food and physical activity is fundamental to addressing this crisis.”
Since TFAH’s first report in 2004, the national adult obesity rate has increased by 37%, and the national youth obesity rate has increased by 42%. Iowa is one of 21 states with an obesity rate over 35%.

“Obesity is somewhat like a tax that society keeps paying year after year after year, and many people might say it’s too expensive to treat obesity,” said Tim Dall, executive director of life sciences for Global Data PLC and the leader of the “Obesity’s Impact on Iowa’s Economy and Labor Force” study. “I think one thing our study shows is that it’s expensive to not treat obesity.”
The Iowa report estimated that 31,400 fewer adults were in the workforce as a result of having obesity or excess weight and that women with obesity experienced 9% reduced earnings, compared to no reduced earnings for men with obesity.
“I think we were surprised at how many fewer adults are in the workforce because of obesity, and especially at a time when there’s high demand for labor,” Dall said. “In some industries, there are shortages of workers, and we really need everyone who’s willing to work, we need them in the workforce. … We estimate about 5,500 premature deaths occur annually. Now, many of these people would have been older and not necessarily in the workforce, but if you look at over the past several years, people who have died, a number of them would have still been working today if not for their premature [death] – people in their 50s, 60s, people kind of in their prime productivity and earning years.
“I think another really surprising factor was that obesity is associated with reduced earnings for employed women at 9% but not for men. There was a study that we reviewed in the literature from South Korea, and they found women with obesity earned 9% less, the identical number we had, but no effect for men.”
The estimates of increased health care costs associated with obesity and excess weight include $619 million for employers and $360 million for households with private insurance; $132.8 million in higher Medicaid costs to Iowa, which accounted for 8% of state Medicaid spending; and $1.1 billion in federal Medicare and Medicaid spending, which were excluded from the overall economic impact number for Iowa to focus on state workforce and budget implications.
“Without addressing obesity, we will continue to pay higher costs for health care,” Dall said. “In addition, for people with obesity and their families, there are implications for their employment levels and their earnings. And that has a ripple effect on state tax collections, income taxes, sales taxes, business taxes. From the perspective of employers, they’re paying more for health insurance for their employees. And also, people with obesity are more likely to have more missed workdays per year being out sick. These are costs to the employer as well as to the employees. I guess one takeaway is that obesity is costing everyone money, even if you don’t have obesity yourself, because that’s less tax revenue that people are paying and just reduced economic activity altogether.”
Beyond the calculable costs of obesity, the chronic health condition also has led to reduced workforce productivity; stigma, bias and discrimination in various aspects of life, including education, employment, health care and relationships; health complications; diminished quality of life; and early mortality, according to the study.
Report recommendations
The “Obesity’s Impact on Iowa’s Economy and Labor Force” report outlines recommendations for state policymakers and employers to increase access to modernized and evidence-based obesity care.
For state policymakers, the report recommends promoting insurance coverage for comprehensive obesity treatment that includes intensive behavioral counseling, nutrition support, pharmacotherapy and bariatric surgery; expanding Medicaid coverage for obesity treatment; and investing in community-based programs and education campaigns.
“State policymakers can invest in community-based programs and infrastructure that serve as an adjunct to access to obesity treatment, ensuring individuals have access to healthy, affordable food and safe, affordable opportunities for being physically active,” according to the report. “Education campaigns can increase awareness about the causes of and health risks associated with obesity and promote evidence-based obesity treatments. Investing in community health worker (CHW) programs, for example, can be a cost-effective way to provide outreach and support to address obesity among underserved populations.”
For employers, the report recommends offering insurance coverage and wellness programs for obesity care at parity with other chronic diseases, fostering a culture of support and inclusion, and providing education and resources.
“Employers can create a culture of support and inclusion that recognizes and accommodates the needs of employees with obesity,” according to the report. “This can involve implementing non-discriminatory policies, offering weight bias and stigma training, creating a supportive workplace environment that promotes healthy behaviors such as providing healthy food options, offering opportunities for physical activity, and providing reasonable workplace accommodations for individuals with obesity and related health conditions.”
One challenge that Dall highlighted is some employers may not have as high of an incentive to invest in their employees’ health due to high turnover rates or simply might not be able to afford good care.
“In general, your larger companies tend to have better benefits and be more engaged in something like this than, say, smaller companies that maybe financially are less likely to be able to afford good benefits for their people, or industries or companies where there’s just kind of high turnover of staff,” he said.
In addition to the recommendations for state policymakers and employers, Dall said resources like the Centers for Disease Control and Prevention and National Institutes of Health offer suggestions for individuals that focus on increasing physical activity levels and gaining better control over a diet. Diet recommendations range from altering the types of foods being eaten, like reducing the amount of processed foods being consumed, to reducing portion sizes.
Additional recommendations include advice on who should receive treatment in the form of pharmacotherapy or bariatric surgery.
“There are a lot of recommendations out there,” Dall said. “The challenge is that not very many people kind of have access to the treatment mostly because of cost. And so even though there are lots of recommendations about who should receive care, a very small proportion are actually receiving that care. But there are many things that individuals can do, and for many people that might be successful, but not everyone can do it on their own, and there are a variety of reasons, many of which are clinical reasons.”
The report also outlines the potential value of treating obesity in terms of health benefits and cost savings in health care expenditure, modeling scenarios of body weight loss up to 5%, 10%, 15%, 20% and 25%.
Over the next 10 years, maintaining a 5% loss of body weight could result in a 33% lower incidence of type 2 diabetes, 11% fewer heart attacks, 16% fewer strokes and a 2.6% reduction in overall mortality,” the study estimates. Sustaining a 25% weight loss could potentially reduce the onset of type 2 diabetes by almost half and reduce the occurrence of cardiovascular conditions by about a third.
For those who successfully achieve a 5% weight loss in the first year, the report estimates an average savings of $332, and if maintained over 10 years, a cumulative medical cost savings of $5,800 per person. Meanwhile, for individuals with a BMI greater than 40 kilograms per square meter, sustaining a higher weight loss can lead to medical cost savings of about $15,500 over the next 10 years.
“Statewide, maintaining a 5% reduction in weight among Iowa adults with obesity could save $3.9 billion in medical costs over the next decade,” according to the report. “Potential savings rise to $9 billion under the scenario of maintaining up to 25% reduction in weight – though many people with obesity will not require the full 25% weight loss to move out of the obesity range.”
Current efforts in Iowa
Hy-Vee Inc. is one company that has already begun to implement strategies in an effort to help prevent and treat obesity. The Hy-Vee Healthy Lifestyles program encourages employees to take a more proactive role in monitoring their health with a “know your numbers” strategy. It focuses on physical, mental and financial health, and employees are encouraged to complete various educational and screening programs throughout the year. Biometric screenings are included in the program and performed by dieticians within the company.
“Knowledge is power when it comes to our employees’ own health, and this program gives our health teams the tools they need to start the conversations with our employees,” said Amy Wadstrom, chief operating officer for Vivid Clear Rx, a subsidiary of Hy-Vee. “Part of that conversation could include discussing programs our Hy-Vee dietitians offer for both employees and patients. The dietitian team offers several programs to help manage obesity, including a weight management program, which allows individuals to prioritize their health and increase their nutritional knowledge during a five-week healthy lifestyle and weight management program.”
Vivid Clear Rx, a pharmacy benefit manager, assists other businesses in developing plans that make clinical and fiscal sense for improving health outcomes within their workforces.
“Employers want to help their employees make the best possible health choices, but the employees have to want to make those changes as well,” Wadstrom said. “It comes down to behavior modification, a supportive environment and providing employees as many tools as possible. As a Hy-Vee company, at Vivid Clear Rx, we’re uniquely positioned to help both employers and employees in this health journey as we can help maximize an employer’s benefit costs and provide the health improvement tools available. We want to be a part of an employee’s lifetime journey to make their lives easier, healthier and happier.”
The Iowa Department of Health and Human Services has also taken on efforts to help in the prevention and treatment of obesity. Collaborating with the Healthy Iowans Partnership, HHS promotes Healthy People 2030 objectives and recommendations in an attempt to improve the health of Iowans, including efforts to address obesity and comorbid conditions. One of those initiatives is the 5-2-1-0 Healthy Choices Count, which promotes evidenced-based healthy eating and active living approaches.
HHS is also part of the Healthiest State Initiative and partners with Healthy Hometown Powered by Wellmark, supporting community initiatives and policies around obesity prevention.
In addition, the Healthy LifeStars and the Iowa Institute of Public Health Research and Policy are working on implementing the Health LifeStars program in Iowa in an effort to end childhood obesity by promoting healthy lifestyle choices. And the Iowa Farm to School and Early Care Coalition is a community-based program that aims to provide children with access to healthy foods.
Other state organizations that are involved in efforts to help prevent and treat obesity include the Iowa Department of Public Health, the Iowa Medical Society and the Iowa Healthcare Collaborative.
“I think there are a variety of ways that we’ve been looking at, ‘How do we address obesity and other diet-related illnesses?’” Jami Haberl, executive director at the Iowa Healthiest State Initiative, said. “Everything from our Double Up Food Bucks giving people access to healthy fruits and vegetables to the Produce Prescription Program. I think even our ‘5-2-1-0 Healthy Choices Count!’ campaign has really focused on helping all of us have a better understanding of healthy habits and really working with our youth to build those healthy habits.
“But then also, ‘How do we set up our environment so that the healthy choice is the easy choice?’ I think that’s a big driver to a lot of our challenges, and then really looking at the mental health component. I think the tie between food and mood, there’s more and more research tied to that, and so just trying to reduce the stigma around mental illness in our state. I think all of it kind of ties together, everything that we’ve been working on for a number of years, getting people to be more active, increasing access to those healthy options and really building an environment so that you have access to those healthy options are all critical components around the obesity conversation.”
Next steps
One of the first steps in response to the newly released findings from the “Obesity’s Impact on Iowa’s Economy and Labor Force” report will be a roundtable discussion presented by Lilly on Oct. 3.
The Iowa Healthiest State Initiative Obesity Roundtable will take place from 9 a.m. to 11 a.m. at the State Historical Building at 600 E. Locust St. in Des Moines. The event is open to the public, and registration can be accessed through the Iowa Healthiest State Initiative website.
Leaders from across the state will have an opportunity to learn about the “Obesity’s Impact on Iowa’s Economy and Labor Force” report and discuss actions to address the impact that obesity has on the state.
“We’ve invited a number of business leaders, government leaders and nonprofit organizations to learn more about the report and then hopefully have dialogue and discussion about where do we go from here now that we understand kind of the economic and workforce impact that it is having on our state today,” Haberl said.
Haberl will provide introductory remarks, followed by a medical perspective from Leon Jons, a clinical associate professor of internal medicine-endocrinology and metabolism at University of Iowa Health Care, and a policy and patient perspective from Catherine Ferguson, vice president of federal advocacy for the American Diabetes Association.
Dall will present on the economic impact of obesity in Iowa, followed by a Q&A and an employer perspective from Wadstrom. The event will also include a pillars panel and action discussion, as well as a conversation about next steps.