Telehealth: What’s changed and what’s next?
More than two years into the pandemic, telehealth innovations are just starting

SARAH BOGAARDS Jun 1, 2022 | 5:53 pm
7 min read time
1,618 wordsBusiness Record Insider, Health and Wellness, Innovation and EntrepreneurshipAfter the initial scaling of telehealth technology and investment in tools and education for providers and patients, local health care organizations have spent the last two years adapting, evaluating and determining their approach to the modality.
MercyOne went from offering telehealth as an option for primary care and a few specialties to now having it available for more than 70 of its specialties. Janell Pittman, MercyOne chief marketing and digital strategy officer, said the health system has incorporated additional digital services like remote patient monitoring to identify changes in conditions as well as tools for virtual diagnostic testing and a new platform that matches patients with a compatible provider.
Des Moines-based startup OpenLoop was founded in early 2020 as a way to increase accessibility of providers by placing physicians in shifts at nearby rural hospitals when they had time in their schedule. By the end of the year it had pivoted its business model to providing the same kind of matching but for telehealth companies that were getting off the ground and needed staff.
The demand for telehealth is no longer at its peak as in-person services have returned, but it remains a popular option among patients for whom it’s convenient and who may face barriers to accessing care without it.
Tracy Liptak, a licensed independent social worker and the clinical director for Optimae Behavioral Health Services in southeastern Iowa, said more patients in rural areas continue to opt for virtual psychiatric medication management services while many in the Des Moines area have returned to an in-person format. Of Optimae’s 7,150 total mental health appointments so far in 2022, 68% have been done using telehealth.
Optimae worked during the pandemic to address the technology divide for rural patients, purchasing tablets with CARES funding and offering computers at their recovery and resource centers that patients could use for telehealth services. Liptak said it was common to hear that patients didn’t have a smartphone or a device equipped for telehealth, whether it was because it wasn’t affordable or there wasn’t reliable access to the internet.
UnityPoint Health’s director of telehealth, Calvin Heller, said the rapid scaling of telehealth has meant expanding the number of specialties available through telehealth and its reach to rural areas. Across Iowa’s rural ZIP codes, UnityPoint served 41% of them via telehealth in 2019, and 90% by the end of 2021.
For patients who don’t have travel or technology barriers, the convenience still matters. Pittman said MercyOne has found telehealth helps patients, especially those with chronic illnesses, schedule and keep appointments.
Matt Dietz, MercyOne division director of digital health, said MercyOne is tracking multiple longitudinal studies, which anecdotally suggest that a telehealth visit decreases the risk of patients canceling or missing an appointment. In MercyOne’s western Iowa market, Dietz said rates of patients missing appointments have decreased by about 30% with the use of telehealth.
Telehealth also brings elements of convenience to the physicians’ role. In fact, that is part of the mission OpenLoop has built its business around.
CEO and co-founder Dr. Jon Lensing said the startup handles administrative tasks for physicians, including licensing and credentials, so they can “focus on what [they] are trained for and want to do, and that’s see and help patients.”
Now that telehealth is an option for many health care providers, Lensing said OpenLoop can support doctors who may be new to the modality and make it possible for them to see patients from across the country on their time.
A similar matching and placement process is happening at Optimae in the local mental health space. Liptak said when there is a cancellation or opening in a provider’s schedule, they have a chance to address another patient’s need without having to travel.
“There’s such a huge need for those services that we were delighted to realize that it’s almost like being able to beam up,” she said. “Sometimes we just wish we could wave a wand and be in a different office where that need was. Now we can do it.”
She said part of the benefit is that Optimae can do more with the providers they have, but she also hopes the flexibility it offers will help attract new workers to the field.
“Being able to say, ‘Oh, I could actually see someone at [6 p.m.].’ … That’s an advantage. Being able to be in different locations, which sometimes can be refreshing and also can allow them to increase their productivity,” she said.
Future of telehealth long term waits to take shape
Iowa’s Public Health Disaster Emergency Proclamation expired in February, but waivers relating to the coverage and practice of telehealth for Medicare and Medicaid patients under the federal proclamation remain in effect.
A key change was the Centers for Medicare and Medicaid Services’ decision to expand the telehealth services covered by the programs. According to the Kaiser Family Foundation, CMS decided that a subset of those expanded services will continue to be covered through December 2023 – or the end of the year that the public health emergency ends, whichever is later – so it and stakeholders can determine whether services should be added for permanent coverage.
One of the waivers allows patients covered by Medicare to receive telehealth care while in their home and lifts the restriction that patients must live in a rural area to qualify for telehealth services. Under the Consolidated Appropriations Act of 2021, these changes will be permanent for mental health and substance use services delivered via telehealth.
Dietz said treating patients where they are located contributes significantly to the convenience factor of telehealth visits, which is one reason why MercyOne is advocating on the state and federal levels and working with the private insurance companies to keep it and some of the other emergency measures in place after the proclamation expires.
The current federal proclamation expires in mid-July, and it is expected to be renewed as the 60-day notice of its expiration promised by the Biden administration has not been announced.
Federal legislation that passed in March determined there will also be a five-month grace period before any policy changes take effect. But barring any additional legislative action before the proclamation expires, the end of the public health emergency will still present an opportunity for variation in the coverage of telehealth services.
Heller said UnityPoint is committed to continuing telehealth services, but it could mean navigating uncertainty and the different ways it is covered by the individual insurance companies as well as the government.
The concern with more variation, he said, is that it could make it “much more challenging to streamline and scale” telehealth delivery.
“I think we have enough momentum going now that [telehealth] will continue, but I think there’s some risk of variation among commercial insurance that could impact patients and consumers and what they have access to,” he said.
Iowa currently requires health insurers to cover telehealth services the same as in-person services. In the 2021 legislative session a bill proposing that all health care providers would receive the same level of reimbursement for telehealth and in-person services failed to pass both chambers, but a later bill passed, creating payment parity for mental health care providers only.
Liptak said maintaining an equal level of reimbursement for telehealth from Medicare and Medicaid and private insurers is “vital” to Optimae’s ability to continue offering the services.
While the full scope of telehealth’s future depends on not-yet determined rules and decisions, she said her vision for Optimae is “for us to be able to use the benefits of technology, including telehealth, in combination with the most individualized and personal level of care.”
Optimae started performing crisis evaluations via telehealth in southeastern Iowa emergency departments where the Optimae provider is based in the same region and able to connect the hospital and patient with other community resources if needed. Liptak said the plan is to continue the service at least into 2023 as it supports hospitals that otherwise don’t have mental health specialists.
Similarly, MercyOne is studying how its inpatient mental health units can use telepsychiatry services to provide outpatient follow-ups in hopes of preventing an acute need for a visit to the emergency department.
Even though telehealth’s role has changed significantly since the pandemic started, it’s uncertain how the landscape will look as organizations are working out what their own approach to telehealth delivery will be. Both MercyOne and UnityPoint are concentrating efforts on gathering data to inform their next steps into telehealth.
Lensing said that what has happened so far is “the first version” of telehealth and that looking forward, there is potential for innovations beyond virtual doctor visits that all stakeholders can contribute to.
He said insurance companies are showing interest in hybrid approaches to care and considering how to maintain convenience in health care, which then supports better outcomes.
Once there is an idea of how the different models of telehealth in Iowa “blend together,” he said synergies and partnerships could develop between organizations, including hospitals and health care startups.
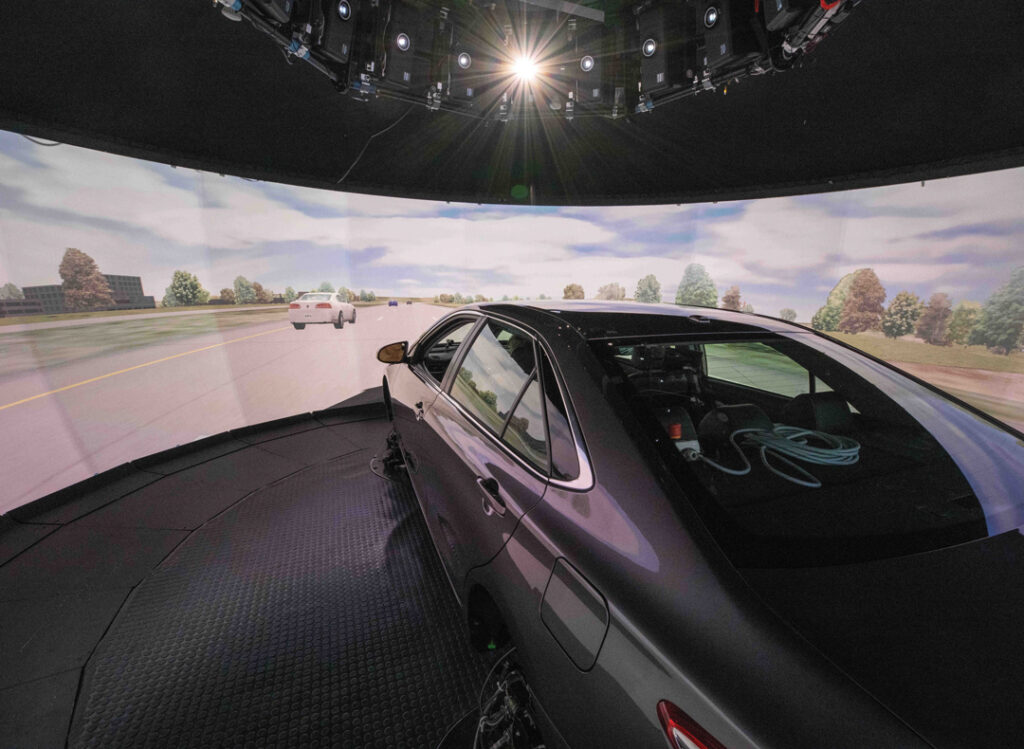
After a few iterations on telehealth, Lensing said he expects it will focus on giving patients digital tools to monitor their health every day and move away from the default of going to see a doctor in person as the first step for care.
“The interesting changes that I think we’re going to be seeing is how to use technology to really enable a true digital health experience,” he said. “We have to take a big step back from making all of your health care done at a hospital and now making it done where a patient is – be that at home, at the workplace, in the car when you’re traveling – just a daily occurrence.”